Heart and Vascular Care
Want to learn more about this at Kettering Health?
What is atrial fibrillation?
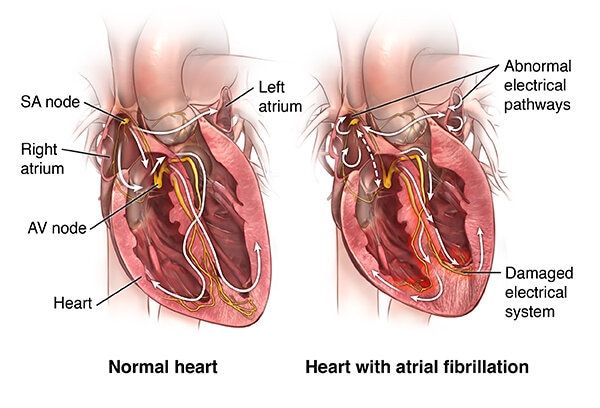
Atrial fibrillation, or AFib, is the most common type of abnormal heart rhythm (arrhythmia).
During AFib, the signal to start the heartbeat is disorganized. This causes the atria to quiver (fibrillate). The disorganized signals are then transmitted to the ventricles. It causes them to contract irregularly and sometimes quickly. The contraction of the atria and the ventricles is no longer coordinated. The amount of blood pumped out to the body will vary with each heartbeat. The ventricles may not be able to pump blood efficiently to the body.
The quivering atria can lead to blood pooling. This pooling can cause blood clots to form inside the heart. Most clots form inside the left atrium. That’s because the left atrium has a pouch (left atrial appendage) in the muscle wall. This pouch is often large with several lobes. Blood can pool and form clots inside the lobes. This increases the risk of forming blood clots. These clots can then be pumped out of the heart and travel to the brain, causing a stroke. This is why AFib greatly increases the risk of stroke.
Doctors don’t fully know the function of this pouch.
Doctors classify AFib in 3 ways:
- Paroxysmal. Sometimes AFib occurs briefly and then goes away on its own. It may last for seconds, minutes, hours, or up to 7 days before returning to a normal rhythm.
- Persistent. This is AFib that does not go away on its own. Treatment may be used to return the heart to a normal rhythm. It lasts for 7 days or longer. AFib that lasts longer than a year is called long-standing persistent atrial fibrillation.
- Permanent. AFib may be called permanent when a decision is made to no longer control the heart’s rhythm, or despite best efforts, normal rhythm can’t be restored.
AFib is common in adults. The risk increases with age. It is more common in men than in women.
What causes atrial fibrillation?
AFib can happen from any type of problem that changes the way the heart handles electricity. Sometimes the cause is unknown. There is a range of things that can increase this risk. Some of the risks include:
- Older age
- High blood pressure
- Coronary artery disease
- Heart failure
- Rheumatic heart disease from a past Streptococcus infection
- Heart valve defects, such as mitral valve prolapse with regurgitation
- Pericarditis
- Congenital heart defects
- Sick sinus syndrome
- Hyperthyroidism
- Obesity
- Diabetes
- Lung disease
- Obstructive sleep apnea
- Metabolic syndrome
- High-dose steroid therapy
AFib is also more likely to happen during an infection or right after surgery. Stress, caffeine, and alcohol may also set off attacks. People who do a lot of repeated vigorous endurance exercises, such as running marathons, can develop atrial fibrillation.
Certain people may be at greater risk of developing AFib. This is because of differences in genes they inherited from their parents. This is not yet fully understood.
Who is at risk for atrial fibrillation?
AF is more common in people who are over 65. It’s also more common in men than women. Underlying heart disease, high blood pressure, thyroid problems, too much alcohol use, sleep apnea, and certain lung diseases put people at risk for atrial fibrillation.
What are the symptoms of atrial fibrillation?
AFib can cause different symptoms. This is especially true when it is not treated. These can include:
- The feeling that your heart is skipping beats or beating too hard (heart palpitations)
- Shortness of breath
- Chest pain
- Dizziness or fainting
- Weakness and tiredness (fatigue)
- Confusion
- Swelling in the feet, ankles, and legs
Sometimes AFib has no symptoms. The first symptom of atrial fibrillation may be symptoms of a stroke.
Call to see if you qualify for a next-day consult
Call (937) 884-1115 to ScheduleHow is atrial fibrillation diagnosed?
Diagnosis starts with a health history and physical exam. An internist or primary care healthcare provider will often makes the diagnosis. You may be sent to a cardiologist for more assessment and treatment.
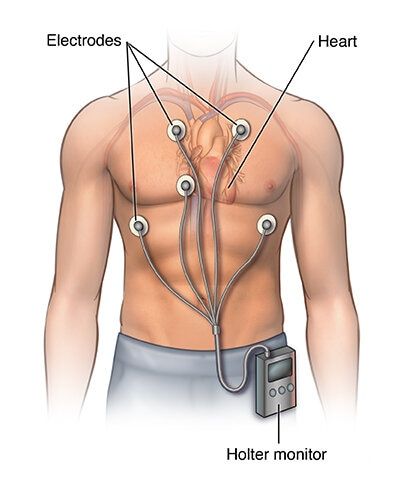
An electrocardiogram (ECG) is very important for a diagnosis. Healthcare providers use this test to study the heart signal and rhythm. In some cases, the diagnosis can be made based on this test alone. If the AFib comes and goes, you might need an electrocardiogram over a longer period with a Holter monitor or an event recorder to pick up the rhythm. Sometimes, you may have a small implanted heart recording device called an implantable loop recorder put under the skin over the heart. This can monitor for AFib over several years.
Other tests might be used to help plan treatment. These might include:
- Echocardiogram, to check the heart’s structure and function
- Cardiac stress testing, to check the blood flow in the heart
- Blood work, to check for thyroid levels, diabetes, and possible health conditions
- Sleep study, when obstructive sleep apnea is suspected
How is atrial fibrillation treated?
Your healthcare providers will work with you to create a specific treatment plan. Treatment options vary according to your health history, your symptoms, and your preferences. Some people who don’t have any symptoms may not need a large amount of treatment. Some general categories of treatment are discussed below.
Medicines
- Blood-thinning (anticoagulant) medicines or aspirin, to help prevent stroke
- Medicines to slow the heartbeat, such as beta-blockers, digoxin, and calcium channel blockers
- Medicines to help prevent AFib (antiarrhythmics)
- Treatment for the main cause of AFib, if known
- Medicines to treat heart failure if present, such as ACE inhibitors
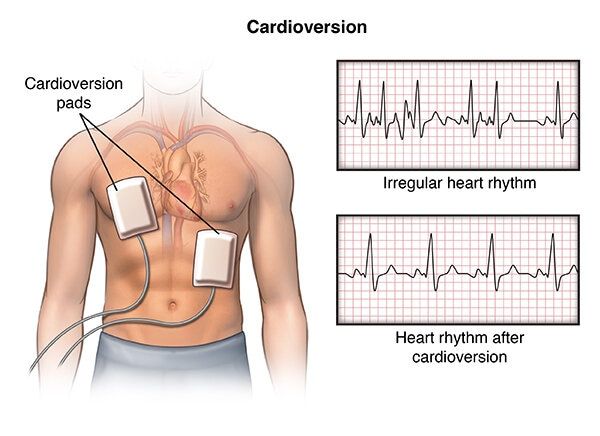
Cardioversion
Before other treatment is started, you may first need a procedure called an electrical cardioversion. This can help get the heart back into a normal rhythm. Your provider uses special pads or paddles to send one or more brief electrical shocks to the heart. This is to stop the signal that is making the atria quiver and reset the heartbeat to normal. You may need a special echocardiogram called a transesophageal echocardiogram. This is to make sure you don’t have a clot in your heart that could cause a stroke if the cardioversion is successful.
Ablation
Procedures such as catheter ablation may be used to restore normal rhythm and improve symptoms if medicines and electrical cardioversion have not worked. Or they may be done if your doctor doesn’t want you to take medicines long term. The catheter passes through a vein leading to the heart to locate the cause of the irregular heart rhythm. Specialists then perform one of three types of ablations, including the following:
- Cryoablation, which involves freezing and scarring the unwanted tissue
- Radiofrequency ablation, which involves burning and scarring the unwanted tissue
- Pulsed field ablation, which involves short bursts of electric energy to target the unwanted tissue
In some cases, the conduction node between the atria and the ventricles (AV node) will be destroyed using catheter ablation. This prevents the problem signals from passing to the ventricles. A pacemaker is then put in to control the heart rate and rhythm in the ventricles.
Surgery
Surgery may be used to restore normal rhythm. During surgery, your healthcare provider may use different methods to create scar tissue in the areas of the heart, causing the abnormal signals. The scar tissue disrupts the abnormal signals and may stop AFib from occurring. Another procedure, called a hybrid surgical-catheter ablation for AFib, may be considered. It combines a surgical approach and a catheter ablation. It allows access to the outside and inside of the heart. Using both approaches may effectively block the abnormal electrical signals.
In the long term, treatment focuses on either controlling the heart rate or preventing the abnormal rhythm.
What are possible complications of atrial fibrillation?
Stroke and heart failure are the major complications of AFib. Blood can pool in the atria during AFib. This can cause a clot. This clot can travel to the brain and block a vessel there, causing a stroke. Blood-thinning medicines help reduce this risk. What you are prescribed will depend on your risk of stroke. If you are at low risk, you may take daily aspirin or sometimes nothing at all. If you are at high risk, you will need a stronger blood thinner.
AFib also sometimes causes heart failure. Because the ventricles are beating so irregularly, they can’t fill normally. The atria also can’t squeeze in the correct way. This also reduces filling in the ventricles. In some cases, this means the heart can’t pump enough blood to the body, causing heart failure. A rapid heart rate in AFib that’s not treated will increase the risk of heart failure. Heart failure is treated with lifestyle changes, medicine, procedures, or surgery. Medicines that lower the heart rate will also help prevent heart failure.
AFib is also linked to an increased risk for dementia and a shorter lifespan.
What can I do to prevent atrial fibrillation?
Controlling risk factors for atrial fibrillation may prevent AFib from developing. This includes managing underlying heart disease, high blood pressure, thyroid problems, sleep apnea, obesity, and lung diseases. Risk factor control also means making healthy lifestyle choices. These choices include eating a healthy diet, exercising regularly, maintaining a healthy weight, and not smoking. Drink alcohol only in moderation, if at all. If you have an alcohol abuse problem, consider getting help.
How can I manage atrial fibrillation?
You will need regular follow-up for your AFib. Blood-thinners called direct-acting oral anticoagulants (DOAC) medicines may be recommended by your healthcare provider to prevent stroke. You don’t need frequent blood tests for these medicines. But you may need to have your kidney function checked periodically.
If you take warfarin, you will need more frequent blood tests. You will also need tests such as a prothrombin time (PT) if you take warfarin. This test measures the time it takes for your blood to clot. It records your reading as an international normalized ratio (INR). Your healthcare provider can change your medicine dose if needed.
Your doctor may advise a device called a left atrial appendage closure to prevent stroke if you can’t take blood-thinners. The device closes off an area in the left atrium where most blood clots form that cause stroke.
There are other steps you can take to help you manage your AFib and maintain a healthy lifestyle.
- Eat about the same amount of certain foods, such as green leafy vegetables, if you are taking warfarin.
- Eat a heart-healthy diet.
- Don’t smoke.
- Be physically active and maintain a healthy weight.
- Keep your cholesterol at healthy levels with lifestyle and medicine.
- Don’t use alcohol or caffeine. They can trigger heart rhythm problems.
- Don’t use certain over-the-counter medicines. They can trigger heart rhythm problems.
- Make sure all your healthcare providers, dentists, and pharmacists know if you are taking a medicine to prevent blood clots.
- If you miss a dose of a blood-thinning medicine, don’t double up your dose. Ask your healthcare provider what you should do.
When should I call my healthcare provider?
Get emergency medical care if you have severe symptoms such as chest pain or sudden shortness of breath. Also, get help if you have signs of severe bleeding.
See your healthcare provider soon if your symptoms are gradually getting worse, or if you have any new mild symptoms or side effects.
Key points about atrial fibrillation
- AFib is the most common abnormal heart rhythm. The atria quiver instead of contracting the way they should. The heart rate usually increases. It is a serious condition, but most people with AFib can lead normal, active lives. You will need to be checked regularly.
- Follow all of your healthcare provider’s instructions about medicines, lifestyle, and monitoring.
- You may be treated with medicine to control your heart rate or rhythm.
- You may need blood-thinning medicine to help prevent a stroke.
- Depending on what blood thinner you take, you may need frequent blood tests and monitoring.
- Go to all your healthcare provider appointments.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also, write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also, know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine, have the test, or undergo the procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Find a Provider who treats Atrial Fibrillation (AFib)
View All Providers-
 Accepting New Patients
Accepting New PatientsZubin
Agarwal, MDCardiac Electrophysiology
Kettering, OH 45429
Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsParthiv R.
Shah, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsHaseeb
Jafri, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsSaleem
Ahmad, MDClinical Cardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsAshwin
Bhirud, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsSameh N.
Khouzam, MDCardiac Electrophysiology
Vandalia, OH 45414
Call to schedule: (937) 454-9527Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsRebecca
Klark, APRN-CNPNurse Practitioner
Kettering, OH 45429
Call to schedule: (866) 224-9472Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsAbram
Basinger, APRN-CNPNurse Practitioner
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -

Jacob D.
Sillaman, PA-CPhysician Assistant
Kettering, OH 45429
View ProfileExisting patient? Log into MyChart