Heart and Vascular Care
Want to learn more about this at Kettering Health?
What is an arrhythmia?
An arrhythmia is an abnormal heart rhythm.
Some arrhythmias can cause problems with contractions of your heart chambers by:
- Not allowing the lower chambers (ventricles) to fill with enough blood, because an abnormal electrical signal is causing your heart to pump too fast or too slow.
- Not allowing enough blood to be pumped out to your body, because an abnormal electrical signal is causing your heart to pump too slowly or too irregularly.
- Not allowing the top chambers (atria) to work properly.
In any of these situations, your body’s vital organs may not get enough blood to meet their needs.
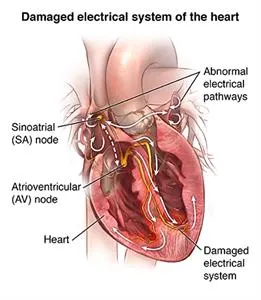
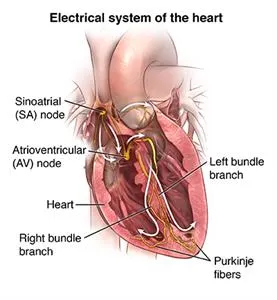
What causes an arrhythmia?
An arrhythmia occurs when there is a problem with the electrical system that is supposed to control a steady heartbeat. With a problem in the electrical system, your heart may beat too fast, too slow, or irregularly.
Who is at risk for an arrhythmia?
Many things can affect the electrical system of your heart and cause an arrhythmia. Substances such as caffeine, alcohol, tobacco, illegal drugs, diet medicines, some herbs, and even prescription medicines can trigger an arrhythmia. Health conditions such as coronary heart disease, high blood pressure, and diabetes raise your risk for arrhythmias. Arrhythmias become more common as you get older.
What are the symptoms of arrhythmias?
The effects on the body are often the same, whether the heartbeat is too fast, too slow, or too irregular. Some symptoms of arrhythmias include:
- A sensation of fluttering or irregular heartbeat (palpitations)
- Weakness
- Tiredness (fatigue)
- Low blood pressure
- Dizziness
- Fainting
- Heart failure
- Collapse and cardiac arrest
- Difficulty feeding (in babies)
The symptoms of an arrhythmia may look like other conditions. Always see your healthcare provider for a diagnosis.
Call to see if you qualify for a next-day consult
Call (937) 884-1115 to ScheduleHow are arrhythmias diagnosed?
Several tests may be used to diagnose arrhythmias. Some of these are discussed below.
Electrocardiogram (ECG) measures the electrical activity of your heart. Small sticky patches called electrodes are placed at specific locations on your body such as your chest, arms, and legs. The electrodes are connected to wires that pick up the heart’s electrical activity and send it to the machine. The machine interprets the activity and makes a graph (tracing). An ECG can show:
- An arrhythmia
- Damage to the heart from a lack of oxygen to the heart muscle (ischemia). This is also called a heart attack (myocardial infarction).
- A problem with one or more of the valves
- Another type of heart condition
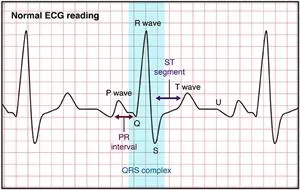
The ECG has several variations:
- Exercise ECG, or stress test. You are attached to the ECG machine as described above. But you walk on a treadmill or pedal a stationary bike while the ECG is recorded. This test is done to check for changes in the ECG during stress, such as exercise.
- Signal-averaged ECG. This procedure is done in the same manner as a regular an ECG, except that your heart’s electrical activity is recorded over a longer period of time, usually 15 to 20 minutes. Signal-averaged ECGs are done when your healthcare provider thinks you may have an arrhythmia, but it’s not seen on a regular ECG. The signal-averaged ECG has more sensitivity to problems in the ventricles called “late potentials.” Signal-averaged ECG is used in research and seldom used in for patients.
- Electrophysiologic studies (EPS). This is a nonsurgical but invasive test in which a small, thin tube (catheter) is put into a large blood vessel in your leg or arm and moved to your heart. This lets your healthcare provider find where the arrhythmia originates within your heart tissue. Your provider can then figure out how to best treat it. Sometimes, your provider can treat the arrhythmia by doing an ablation at the time of the study.
- Holter monitor. A Holter monitor is a continuous ECG recording done over a period of 24 or more hours. Electrodes are attached to your chest and connected to a small portable ECG recorder by lead wires. Holter monitoring may be done when your healthcare provider thinks you may have an arrhythmia. Arrhythmias may last only a very short time and not be seen on during the shorter recording time of a regular ECG. While wearing a Holter monitor, you can go about your daily activities. But you should not do activities that cause a lot of sweating. This could cause the electrodes to become loose or fall off. You should also not take a shower or swim while wearing a a Holter monitor.
- Event monitor. This is similar to a Holter monitor, except that you start the ECG recording only when you feel symptoms. Event monitors are typically worn longer than Holter monitors. You can remove the monitor to shower or bathe.
- Mobile cardiac monitoring. This is similar to Holter and event monitors. The ECG is checked constantly to spot arrhythmias. The ECG is recorded and sent to your healthcare provider regardless of whether you have symptoms. You can also start recordings yourself when you have symptoms. These monitors can be worn up to 30 days.
- Implantable loop recorder. This is a miniature heart recording device that is implanted underneath the skin over your heart. It can record the heart rhythm for up to 3 years. It is useful in diagnosing arrhythmias that happen only now and then or rarely..
How is an arrhythmia treated?
Some arrhythmias may cause few, if any, problems. In this case, you may not need treatment. When the arrhythmia causes symptoms, you have several different choices for treatment. Your healthcare provider will discuss your treatment options with you. Together you will choose a treatment that is best for you. The choice will be based on the type of arrhythmia you have, how severe your symptoms are, and if you have other conditions such as diabetes, kidney failure, or heart failure. These can affect the course of the treatment.
Some treatments for arrhythmias include:
- Lifestyle changes. Stress, caffeine, and alcohol can cause arrhythmias. Your healthcare provider may advise you to not have caffeine, alcohol, or any other things that may be causing the problem. If your provider thinks that stress is a cause, they may suggest meditation, stress-management classes, an exercise program, or psychotherapy to ease stress.
- Medicine. Medicine can treat arrhythmias. The medicine used will be based on to the type of arrhythmia you have, whether you have other health conditions, and whether you take other medicines. Medicines may be used to slow down a fast arrhythmia or lower your chances for a stroke by keeping blood clots from forming.
- Cardioversion. In this procedure, the healthcare provider sends an electrical shock to your heart through the chest. This may stop certain very fast arrhythmias such as atrial fibrillation, supraventricular tachycardia, or atrial flutter. You are connected to an ECG monitor, which is also connected to the defibrillator. The electrical shock is given at a point during the ECG cycle to change the rhythm to a normal one.
- Ablation. This is an invasive but nonsurgical procedure done in the electrophysiology lab. The healthcare provider puts a thin, flexible tube (catheter) into your heart through a large blood vessel in your groin or arm. The provider may use high-frequency radio waves to heat the tissue at the site of the arrhythmia and destroy it. This method is called radiofrequency ablation. Cryoablation is another method that can be used. For this, an ultra-cold substance is put on the site. This freezes and destroys the tissue .
- Pacemaker. A permanent pacemaker is a small device that is put under the skin, often in the chest region just under the collarbone. It sends electrical signals to control a slow heartbeat. A permanent pacemaker may be used to make the heart beat if the heart’s natural pacemaker (the SA node) is not working as it should, or if the electrical pathways are blocked. Pacemakers are often used for slow arrhythmias such as sinus bradycardia, sick sinus syndrome, or heart block.
- Implantable cardioverter defibrillator (ICD). An ICD is a small device similar to a pacemaker. It is put under the skin, often just under the collarbone. An ICD senses the heart rhythm. When the device detects an abnormal rhythm, , it sends an electrical shock to the heart. This corrects the rhythm to a more normal heart rhythm. Some ICDs can act as a pacemaker to send an electrical signal to adjust a slow heart rate. ICDs are often used for life-threatening fast arrhythmias such as ventricular tachycardia or ventricular fibrillation.
- Surgery. Surgery is usually done only when all other treatments have failed. Surgical ablation is major surgery that needs general anesthesia. The surgeon opens your chest to reach your heart. The surgeon destroys or removes the tissue causing the arrhythmia.
What are possible complications of an arrhythmia?
Some arrhythmias have no complications. But arrhythmias that are more serious can cause heart failure, stroke, or even cardiac arrest.
Living with an arrhythmia
Living with an arrhythmia includes making lifestyle changes such as not having caffeine, alcohol, or other triggers. It also includes taking medicines as directed. It may also include having a pacemaker or ICD inserted. If you have a pacemaker or ICD, ask your healthcare providers about any limits or lifestyle changes you may need to make. Working with your healthcare provider can promote your health and well-being.
When should I call my healthcare provider?
Tell your healthcare provider if:
- Your symptoms get worse or you start to have new symptoms
- You have side effects from your medicine
- You need help with managing stress or emotions
Key points about arrhythmias
An arrhythmia is an abnormal heart rhythm.
- An arrhythmia can occur in the sinus node, the atria, or the atrioventricular node, or the ventricle.
- Some arrhythmias cause few, if any, problems.
- Other arrhythmias can cause serious complications such as heart failure, stroke, or even cardiac arrest.
- Many treatment options are available to treat arrhythmia, including medicines, devices, cardiac ablation, and surgery. Many arrhythmias can be controlled with procedures.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Find a Provider who treats Arrhythmias
View All Providers-
 Accepting New Patients
Accepting New PatientsZubin
Agarwal, MDCardiac Electrophysiology
Kettering, OH 45429
Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsSameh N.
Khouzam, MDCardiac Electrophysiology
Vandalia, OH 45414
Call to schedule: (937) 454-9527Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsParthiv R.
Shah, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsHaseeb
Jafri, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsSaleem
Ahmad, MDClinical Cardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsAshwin
Bhirud, MDCardiac Electrophysiology
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsAbram
Basinger, APRN-CNPNurse Practitioner
Kettering, OH 45429
Call to schedule: (937) 433-2051Existing patient? Log into MyChart -
 Accepting New Patients
Accepting New PatientsRebecca
Klark, APRN-CNPNurse Practitioner
Kettering, OH 45429
Call to schedule: (866) 224-9472Existing patient? Log into MyChart -

Jacob D.
Sillaman, PA-CPhysician Assistant
Kettering, OH 45429
View ProfileExisting patient? Log into MyChart