Gastroenterology
Want to learn more about this at Kettering Health?
The term “acid reflux” might conjure images of people in antacid commercials reaching for a bottle of TUMS on their bedside table, heartburn robbing them of sleep. While this may resonate with many gastroesophageal reflux disease (GERD) sufferers, it may not paint an accurate picture for all.
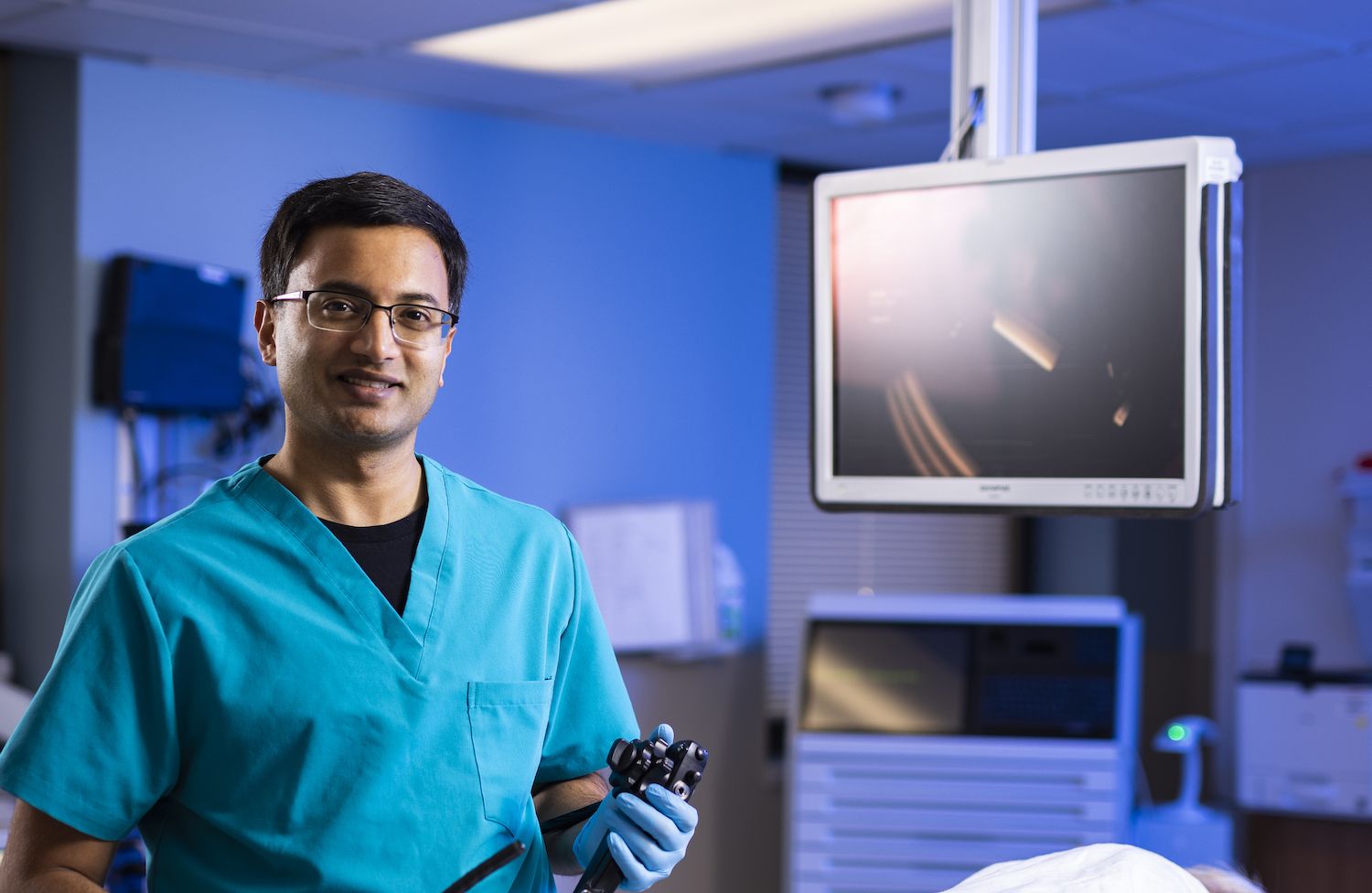
“GERD, by definition, is reflux of the gastric contents from the stomach to the esophagus,” said Dr. Shashank Sarvepalli, a gastroenterologist with specialized training in motility disorders, such as GERD and gastroparesis.
Those with GERD may not always feel the acid rising in their throats. GERD can show up as a multitude of symptoms that can leave people scratching their heads, not even considering reflux.
Atypical symptoms of GERD
While heartburn is often the first symptom that comes to mind, some less typical symptoms of GERD can disguise themselves as other conditions. Atypical symptoms include
- Chest pain
- Respiratory conditions, like asthma, persistent cough, or pneumonia
- Throat problems, ranging from damaged vocal cords, hoarseness of the voice, excessive clearing of the throat, and the sensation of food being stuck in the throat
- Dental erosion
- Trouble sleeping
Patients experiencing any of these systems without relief may want to consider being evaluated for acid reflux.
Dr. Sarvepalli stresses seeing the appropriate specialist for these symptoms first to rule out any other issues. Those with asthma-like symptoms should first see a pulmonologist, and chest pain should be addressed by a cardiologist.
“If they don’t have a clear reason for the symptoms, we can investigate if reflux can be contributing,” says Dr. Sarvepalli. “But the first line of evaluation should be by that specialty.”
Treated just the same
Treatment for GERD is the same, regardless of the symptoms. Treatment aims to address the root of the problem rather than relieve the symptoms.
“We start with lifestyle changes first and foremost,” says Dr. Sarvepalli. These can include
- Losing weight
- Discontinuing the use of tobacco products
- Reducing or avoiding alcohol
- Identifying and avoiding trigger foods
- Avoiding large meals three hours before bedtime
- Increasing physical activity
There is even a breathing technique, called diaphragmatic breathing, that can help you reduce reflux.
If these changes don’t address the issue, acid-suppressing medication, like proton pump inhibitors and H2 blockers, can reduce the amount of acid in your stomach. And while antacids like TUMS or Rolaids may provide temporary relief, they don’t block the production of more acid, so they aren’t a long-term solution.
Finally, surgery may benefit patients who don’t see improvement with medication.
Screening saves lives
Regardless of how GERD shows up, those suffering from chronic reflux should be aware of their risk for Barrett’s esophagus, damage to the esophagus that increases the risk of esophageal cancer.
Screening for Barrett’s esophagus with upper endoscopy is recommended for anyone experiencing chronic reflux for more than five years with three or more of the following risk factors:
- White
- Male
- Age 50 or older
- Family history of Barrett’s esophagus or esophageal cancer
- Smoking
- Obesity
Often, the screening endoscopy can occur at the same time as a colonoscopy.
“There’s a lot of information around colon cancer screening, breast cancer screening, and so on. We’re only starting to understand Barrett’s esophagus,” says Dr. Sarvepalli. “Even though esophageal cancer is less common than breast cancer or colon cancer, it is the second deadliest cancer.”