In late June 2023, Kristy Gilmore was over Ohio’s heat and humidity. And she was ready to meet her baby—even though she had five more weeks. She even prayed, asking God to hurry things along. “Honestly, Kristy says, “labor and delivery sounded better than more waiting.”
But with Phillip, her husband, she learned a new prayer—asking for their baby to arrive at the right time, in the right place, with the right people.

Just a dream
Throughout the previous eight months, Kristy remained calm, cool, and collected. Being a registered nurse (RN) helped, though her expertise was in oncology. She spent most of her time at Kettering Health’s cancer centers as a nurse professional development specialist. Phillip, a college golf coach, knew nothing about healthcare.
So when a nightmare about their baby jolted him, and Kristy, awake, they had different reactions. “Stop there,” she told him with heavy eyelids. “You’re crazy.” Baby and mom were healthy.
But Phillip, wide-eyed and wired, insisted. He wanted to talk about what Kristy wanted during the birth. Her hopes—to see their baby enter the world. And her fears—needing a C-section.
A growing storm
Leaving Soin Medical Center on July 20, having been induced that morning, Kristy had to do more waiting. “My body wasn’t ready,” she says. So they drove home.
Kristy woke up from a nap a few hours later, her back and belly tight with cramping. She hobbled to the bathroom. There, her water broke. She labored at home for a few hours before they left for Soin Medical Center just before midnight.
Thankfully, the late hour—and a tornado watch—made traffic nonexistent. The chaotic sky surrounded their lonely care as Kristy’s contractions intensified.
After settling into a delivery room, Kristy’s birth plan unfolded in textbook fashion. “I labored easily. Dilated easily.”
But Kristy wanted no one to know she was a nurse. Her fear, what she called “the nurse curse,” was that she’d be treated as an RN—not a mom-to-be.
Kristy started pushing. And pushing. And pushing. With no progress. After three hours, her midwife recommended a break.
Then Kristy spiked a fever. She watched her heart rate—and the baby’s—climb. And the room’s momentum shifted. “My nurse kept coming in and out,” Kristy says. “My midwife and the OB-GYN stepped into the hallway.”
Reading the chirping monitors, Kristy asked questions. Jen Phelps, RN, watched Kristy interpret the scribbles and numbers and asked her, “What do you do for a living?”
“Well,” Kristy replied, “I’m a nurse.”
“I could tell,” Jen replied.
Kristy’s fear of “nurse curse” soon lifted, replaced by Jen’s clarity and warmth. “They didn’t treat me any differently,” Kristy recalls. “It was all in my head.”
When things went south

Kristy learned that she needed a C-section—a fear now realized. Feverish and nauseated, she had little energy to respond. Though Phillip knew Kristy’s birth plan, watching her and the baby’s condition plummet, he “made the decision to get the baby out.”
Twenty people filled the room. Each person’s movement precise and calculated, fluid and familiar—”like a dance,” Kristy says. Amid the synchronized surgery prep, Jen “slowed things down to make sure we understood what was happening.”
But the surgery, which started around 8 p.m., soon faced challenges. The baby, not only breech, had flipped sideways, making delivery more difficult. Then Kristy began to hemorrhage blood.
She needed to be sedated. She begged the anesthesiologist not to. But Kristy was losing a lot of blood—nearly two liters by the end of the surgery.
Darcy Fortman, RN, walked Phillip from the operating room. The doors swinging closed behind him, Kristy drifted to sleep. And the care team enveloped her.
Meeting her
Kristy woke up at 4 a.m.
Through groggy eyes, she saw no one. “My husband wasn’t there. My baby wasn’t there.” she then turned to see a nurse, Jen Till, RN, next to her, monitoring Kristy’s blood transfusion.
“I’m so scared,” Kristy whispered.
“I’m not going anywhere,” Jen T. replied.
She explained that Phillip had stepped out. And that their baby was recovering in the Special Care Nursery.
“They’re OK,” Jen T. says. “You’re both OK.”
Phillip walked into the room to see Kristy awake. Sitting with her, he showed her a video on his phone. Kristy watched as their baby—their daughter—took fragile breaths, helped by a CPAP machine. She really was OK.
Thirty minutes later, with help, Kristy journeyed to the Special Care Nursery. There, she met her Edna Joy, “EJ” for short.
Finally here
EJ joined Kristy two days later. As Kristy recovered, she learned more about the C-section, the blood loss, and how the nurses kept Phillip updated and involved while she was sedated. The golf coach even felt a part of Kristy’s care team. “I’m surprised he hasn’t gone back there with a nursing badge,” she says.
As Kristy held EJ, the trauma of her birth fell away. “There was something about holding EJ,” Kristy says. “I didn’t care about what happened.” She was here—despite any impatience and imploded plans.
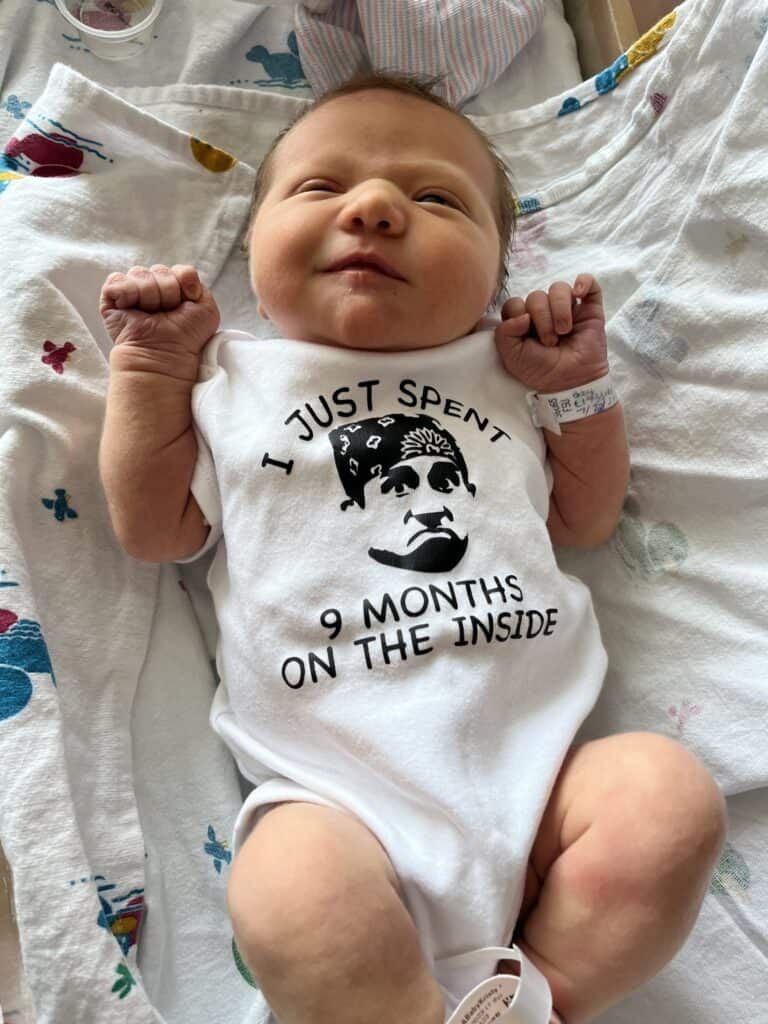
Well, except for the The Office onesie EJ wore home. That, at least, went according to plan.



