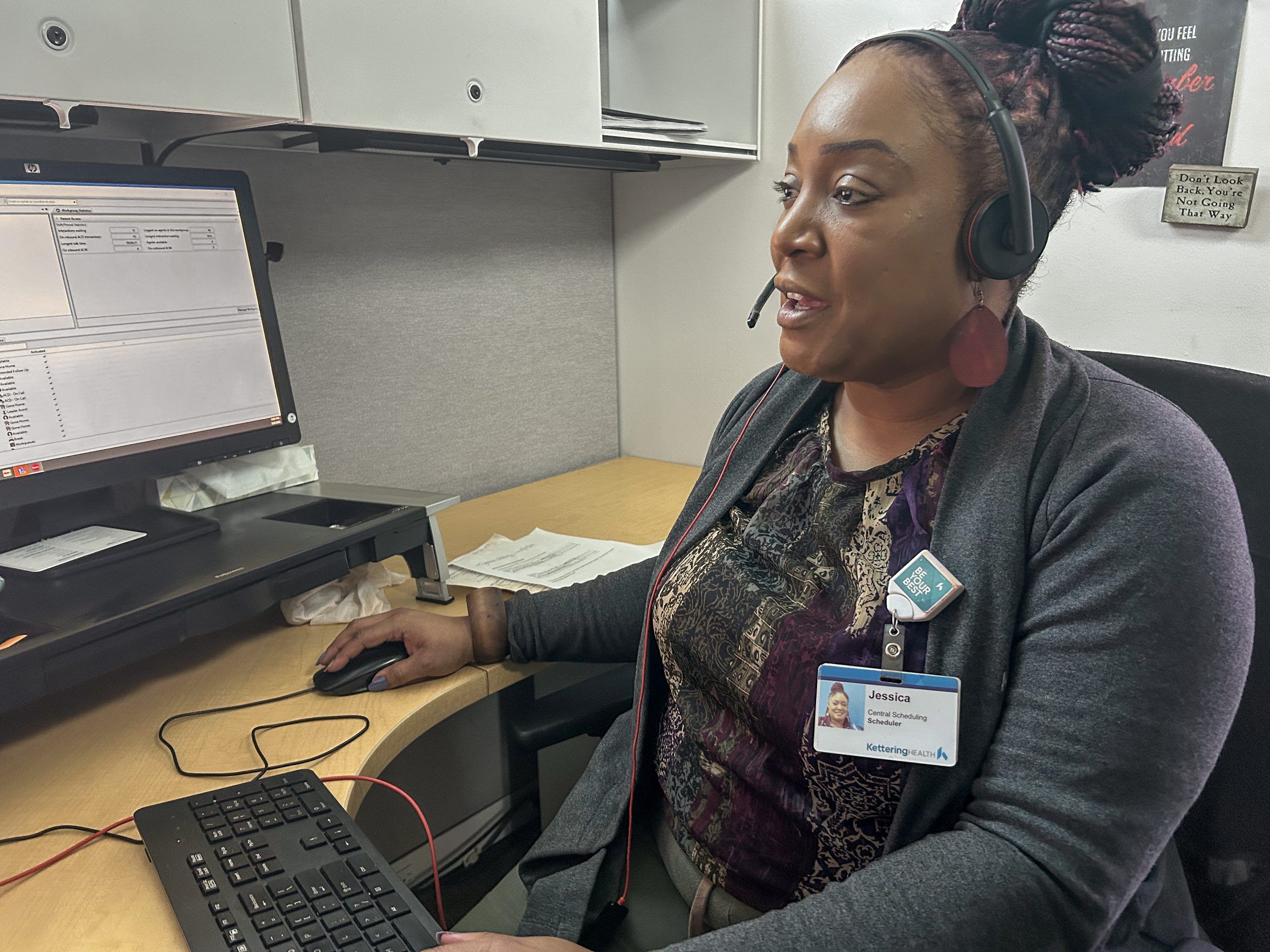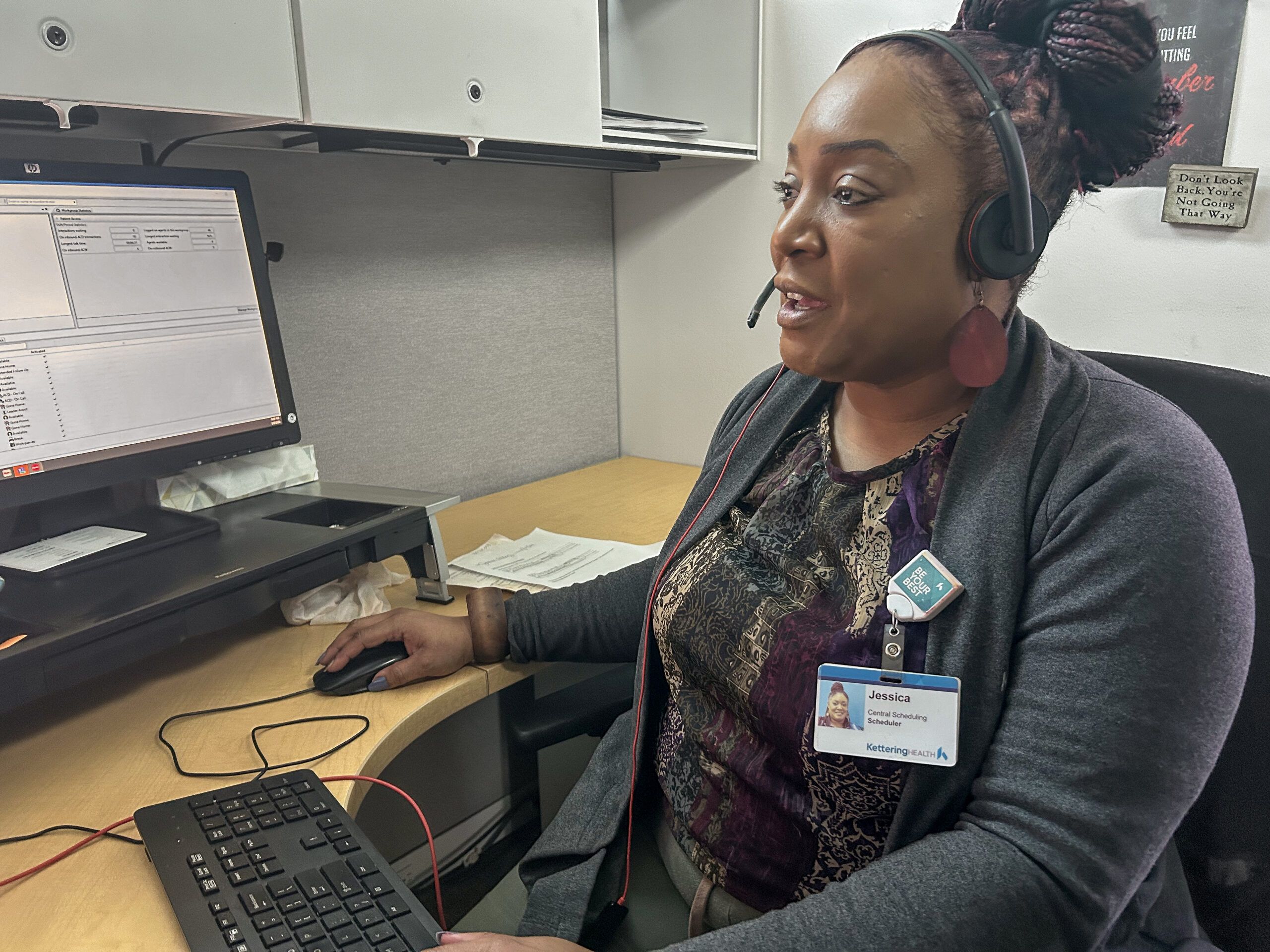
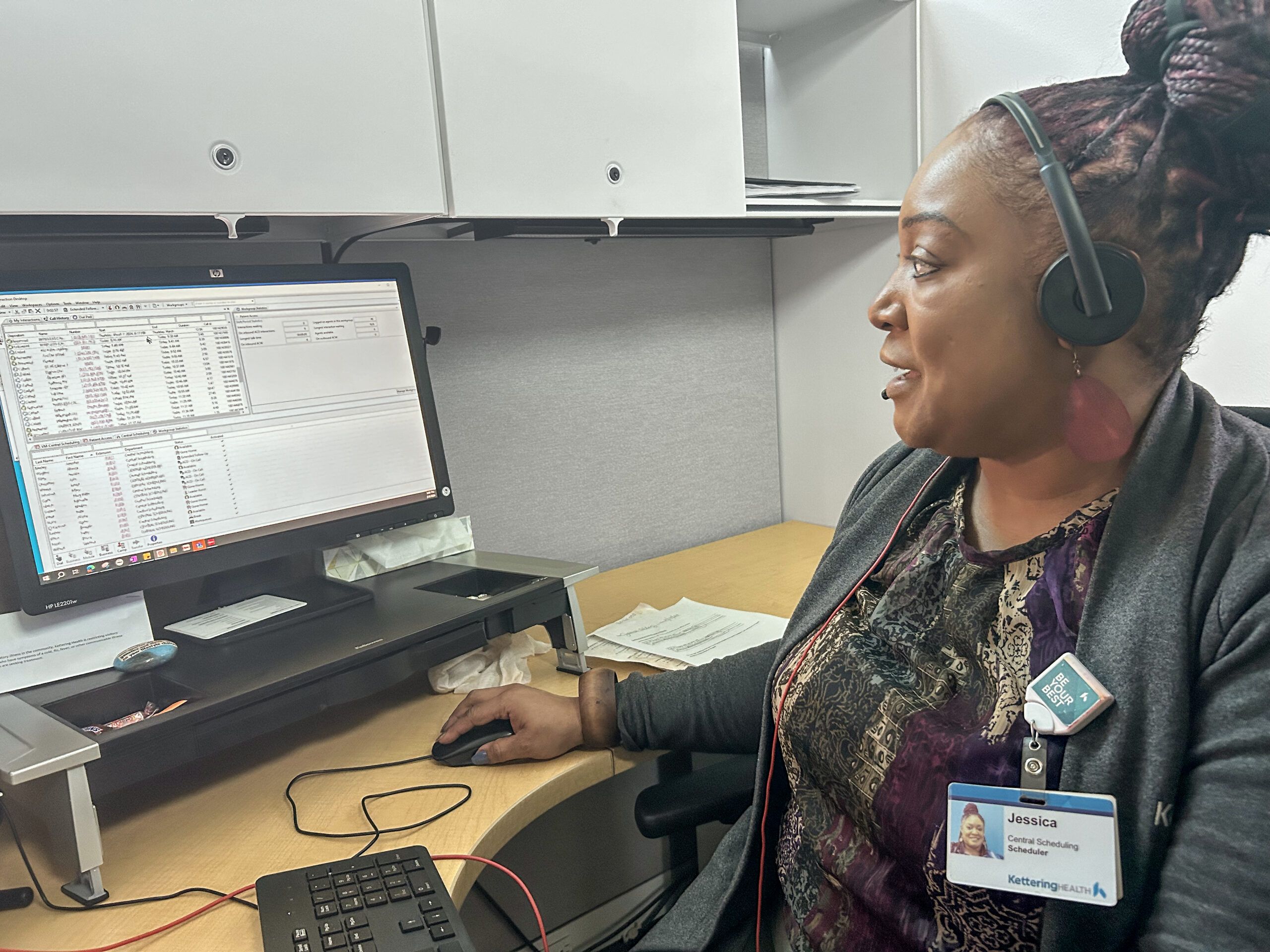
Her operator number is 16. But by the end of her calls, people know her as Jessica.
And while she’s worked in Central Scheduling for only 15 months, she already feels at home. “I’ve been a teacher, a truck driver, even a drug and alcohol counselor,” Jessica Tilley says. “But here, I love it.”
She’s come up with her own catchphrase, too: “One call, that’s all.”
For Jessica, it’s something of a mission statement. She knows that whenever she answers a call, she’s introducing herself to someone needing help. And she aims to meet that need every time on every call.
For most of the 80 to 90 calls she answers between 10 a.m. and 6:30 p.m., she’s helping schedule physician-referred appointments or ordered tests. But not every call is so straightforward.
People often call with questions she’s not prepared for—like how to understand a nuclear imaging test. But that doesn’t stop Jessica from trying to help.
“I Googled that for one person who was nervous,” Jessica recalls. “And I read it to them to try to calm their nerves.”
That’s because “one call, that’s all” is also a philosophy of life. Jessica recognizes that her interactions aren’t with nameless voices. They’re people. People who call confused and upset, their minds racing with worst-case scenarios. Or they call because they’re unfamiliar and intimidated with certain medical phrases—or even the English language.
Sometimes, they call before everything turns upside down.
Taking one more call
By 5 p.m. most days, Jessica craves something sweet. Her go-to solution: the Oreo chocolate pudding from the café on the first floor of the Prestige building.
But before she took her break on January 11, she saw a call waiting in the queue. So she picked up.
“Thank you for choosing Kettering Health Central Scheduling. My name is Jessica. How may I help you?”
“Yea, my name is Josh . . . “
Josh Taziers, 45, had been dealing with breathing issues. And passing out. He recently saw his doctor and was convinced they’d ordered a blood test. But Jessica saw no order.
“Josh sounded frustrated, even a bit angry,” Jessica recalls.
A frenetic back-and-forth spun up, with Jessica keeping the tension at bay using the ICARE customer-service approach. She keeps a printout of it on her desk. “Because I do care,” regardless of someone’s tone, including Josh’s.
Beneath Josh’s tangled tone, Jessica sensed confusion, worry, and a little fear. “I decided to call his doctor and merge the call with Josh.”
A nurse aide picked up. Jessica caught her up on Josh’s questions. But Jessica also noticed a change, specifically with Josh. He’d grown quiet. And his breathing, now short and stunted, sounded like he wanted to say something but couldn’t.
“Josh?” Jessica asked. “Do you want to ask something?”
“Josh?” You there?”
“We’ll follow back up,” Jessica told the nurse aide.
Jessica listened to the momentary silence. Then she heard it again: Josh’s stilted gasps. Jessica tried again to see if Josh might reply.
“Josh, I can hear you breathing. I can hear you in the background. Are you there?”
“Josh, I’m still here. I’m not sure what’s going on. I’m going to call 911.”
Then Jessica heard the muffled thud of something hit the ground.
“I need help”
Jessica felt full-scale worry replace her confusion. But she stayed calm. “Normally,” Jessica says, “something like this would make me panic. But I knew I couldn’t do that.”
She dialed Riverside police, asking for a wellness check at Josh’s address. She stayed on the phone with Josh, who was still unresponsive.
“Josh, they’re coming.”
“I need help,” Josh finally whispered.
“Help is on the way, Josh.”
Seconds slipped into what felt like helpless hours. But it had only been two minutes. Jessica was about to call 911 again when she heard a rush of voices come through on Josh’s line. A paramedic picked up the phone. Jessica told her what she’d heard during the call and stayed on the line, referencing Josh’s chart to make sure the paramedics knew of Josh’s previous hospital visits and medications.
She admits going into a patient’s chart is atypical for someone in Central Scheduling. But in that moment, Josh’s safety was paramount.
“She [the paramedic] told me they would never have known what had happened to Josh if I hadn’t stayed on the call,” Jessica says.
The call ended. The paramedics took Josh to a nearby hospital. And Jessica tried to take her break, but she couldn’t stop worrying about Josh.
The next morning, as she sat down at her desk, Jessica waited to answer her first call. Instead, she made one—to Josh, who was discharged earlier that morning.

They talked about what had happened after their call, along with next steps for Josh and his health. Jessica learned he’d collapsed from a seizure and that he didn’t remember much from their call. What he does remember, though, was Jessica’s clarity and calmness.
“She didn’t trip my nervous system into a worse response,” Josh says. “She was an awesome lady.”
Before their call ended, Josh had something to say.
“He told me, ‘I can’t believe you stayed on the phone with me. You saved my life. Thank you.’”
Jessica doesn’t quite see it that way. “I don’t look at it like I saved his life. I just got him the help he needed.”
Care starts on the phone
When Jessica Tilley, operator #16, answers a call in Central Scheduling, she does so with a singular commitment: to help the caller any way she can with as much humanity as she has.
“I hope to give them an experience,” she says, “where they get the help they need. And maybe even have their frowns turned upside down.”
She guesses that about half of her calls end that way, with some sort of change in the caller. Some sound calmer. Others, more confident. Most are grateful, thanking Jessica by name.
And, on at least one occasion, a caller learned that at Kettering Health, patient care happens not only at bedsides and in ORs, but also over the phone. As Jessica likes to say, “One call, that’s all.”